Travel Checklist
Once your appointment at Ratchaphruek Hospital has been confirmed, our medical travel team will send you a package of important information you need to know before traveling. To help you better prepare your medical travel itinerary, please take a look at this travel checklist. Travel Advice and Assessment before Medical and Surgical Care
Section I: Traveling by Air
In general, if you have the below conditions; it is prohibited to travel by air
- Individuals with health problems are advised to consult a doctor before traveling in order to minimize associated risks. It is also recommended that they carry their personal medication in their carry-on luggage.
– Passengers with disabilities who require assistance during the flight should be accompanied by a designated companion. They should inform the flight attendant in advance about their assistance needs.
– Patients who have received medical treatment and are in stable condition, or those who may experience deterioration during the trip, must submit a travel authorization document (Medical Information Form) to the airline before booking a seat. They should also specify the amount of oxygen required on board, if applicable. The airline reserves the right to refuse travel or request a postponement if the patient’s condition is deemed unsafe. The airline may also require changes in travel arrangements, such as seat configuration or oxygen consumption, or insist on the presence of a doctor and/or nurse to accompany the patient.
– Newborn babies under 7 days old are susceptible to changes in air pressure during the flight. Similarly, premature babies require special considerations. Therefore, a travel authorization document (Medical Information Form) must be submitted for both cases in order to comply with the airline’s policies.
– Pregnant women without any health problems are generally allowed to travel by plane. However, it is advisable to avoid frequent air travel during the early stages of pregnancy due to the potential risks associated with lower oxygen levels on board, which can pose a risk to the fetus. The airline has established regulations for pregnant women as follows:
1. Pregnant women beyond 28 weeks of gestational age must possess a medical certificate stating their expected delivery schedule. This certificate ensures both their safety and the safety of the travel arrangements.
2. For normal pregnancies and pregnancies without twins, air travel is permitted until 36 weeks of gestation if the flight duration is within 4 hours. If the flight duration exceeds 4 hours, travel is permitted until 34 weeks of pregnancy.
3. Pregnant women with twin pregnancies or complications such as placenta previa or a history of premature birth are generally advised not to undertake long-distance air travel. However, if a travel authorization document (Medical Information Form) has been requested and approved, exceptions may be made.
4. Pregnant women beyond 36 weeks of gestation will not be allowed to board the aircraft for safety reasons.
People with heart and respiratory problems
Patients who are not fit to travel by plane are as follows:
1. Patients with uncontrolled chest pain
2. Patients with ischemic heart disease heart failure or chronic heart failure must have normal symptoms able to perform normal daily life without chest pain not panting or no irregular heartbeat In general, it is best to wait at least 4-6 weeks, but if necessary, it is possible to travel after 2-3 weeks of symptoms, but must be under medical supervision and must inform the airline for oxygen if necessary.
3. Patients undergoing coronary artery bypass surgery Do not travel within 2 weeks after surgery to wait for the air in the chest during surgery to be completely absorbed.
4. Heart failure
5. Uncontrolled hypertension (upper pressure over 160 mmHg) patients with hypertension Able to travel if treated first and should prepare medicines suitable for travel and time has changed
6. Untreated irregular heartbeat no blood thinning medication or waiting for pacemaker implantation
7. Abnormal heart valve disease and have shortness of breath
8. Those who go scuba diving or illness caused by reduced pressure Decompression sickness must wait at least 24 hours after stopping diving or after recovering before flying.
9. Leaky lung disease that has not been treated or treated but the symptoms are not stable. And there may be a leak during the machine.
10. Untreated pleural effusion
11. Patients with asthma If there are still severe symptoms The symptoms are still unstable. Or just discharged from the hospital should not travel. 12. Patients with chronic obstructive pulmonary disease. Able to travel if there is no shortness of breath, shallow breathing when walking or when climbing stairs But when traveling by plane there is a problem of insufficient oxygen on board. Pulmonary oxygen pressure should be checked before flying. to ask for more oxygen during the journey
13. Respiratory failure
14. Tiredness, panting while not exercising or have chronic and severe lung problems
15. Lung disease requiring mechanical ventilation or whose symptoms are still unstable for travel
16. Muscle weakness that prevents breathing on its own and must use a ventilator
17. Pneumonia that is still infectious
18. Pulmonary tuberculosis, especially in immunocompromised patients who have been treated for less than 15 days.
– If you have implantable cardiac devices such as defibrillators, cardiac synchronization therapy devices (CRT), implanted cardiac pacemakers (PPM), or use artificial joints, it is important to consult with your doctor before flying. Additionally, remember to carry a medical certificate with you. It is also required to have your personal device identification with you at all times.
– If you require oxygen during your flight, it is necessary to notify the airline in advance. This can be done by completing a medical information form that includes your current clinical condition and the reasons for needing oxygen. Submit the form to the airline for approval, which may take 3-5 working days depending on the airline’s procedures.
Patients with brain diseases or abnormal cerebrovascular conditions:
1. Patients with epilepsy whose symptoms are not under control or those who have undergone brain surgery within the past two weeks without complications should avoid traveling. If travel is necessary, the treating physician may need to adjust anticonvulsant medication to a higher dose for preventive measures. This is because the reduced oxygen levels on board the aircraft can lead to hypoxia, making seizures more likely, especially when combined with travel exhaustion, anxiety, or changes in time zones.
2. Individuals with uncomplicated cerebrovascular disease may face difficulties during air travel due to reduced oxygen supply to the brain cells. The depletion of oxygen levels during the flight can exacerbate their condition and pose a potential risk. It is recommended that patients have their brain symptoms resolved or stabilized for at least two weeks before undertaking air travel. The treating physician should also be consulted to consider the possibility of arranging for additional oxygen on board.
3. Patients who have experienced a recent concussion (within the past 15 days) from an accident should refrain from traveling by air.
4. Individuals with untreated hydrocephalus or who have undergone cerebrospinal fluid puncture within the past week should avoid air travel to prevent any potential leakage of cerebrospinal fluid.
5. Those who have received cerebral angiography within the past three days to examine the blood vessels in the brain should postpone air travel for the time being.
6. For patients with psychiatric diseases, if symptoms are still not under control, travel may not be advisable. If treatment has been successful and symptoms are stable, the patient should be accompanied by a physician, nurse, or a responsible family member who can provide supervision during the trip. The treating psychiatrist must certify that the patient is in a calm state and it is safe for them to travel by plane. In some cases, the doctor may need to administer a sedative or recommend pre-travel sedation for the safety of the patient and other passengers.
Please note that these guidelines are subject to the advice of the treating physician and individual circumstances.
Patients with gastrointestinal diseases:
1. Patients who have undergone abdominal surgery should be aware of the potential for gas expansion in the gastrointestinal tract during air travel. This expansion can pose a risk of surgical rupture. If there are no complications, it is recommended to wait at least 2 weeks after surgery before traveling to allow sufficient time for the gas in the abdomen to be absorbed.
2. Patients with a colostomy (opening of the colon in the abdomen) should ensure they are prepared by carrying an increased number of colostomy bags for replacement during travel.
3. Individuals with bowel obstruction, gastrointestinal tract bleeding, or ruptured esophageal aneurysms should refrain from air travel due to the potential complications associated with these conditions.
4. Patients experiencing severe vomiting or diarrhea should avoid traveling by air until their symptoms are under control, as these conditions can be exacerbated during the flight.
5. Patients who have recently experienced significant blood loss from gastric ulcers should ensure that their bleeding has been effectively stopped and their hemoglobin concentration is above 10 g/dl before considering air travel.
6. Patients who have undergone gastrointestinal surgery within the past 7 days should delay air travel to allow for proper healing and recovery.
7. Individuals who have undergone a colonoscopy within the past 24 hours should avoid air travel due to the potential risks and discomfort associated with the procedure.
Patients with venous thrombosis in the legs:
Sitting in a cramped seat for extended periods during air travel can lead to poor blood flow from the legs to the heart, resulting in swollen feet and legs. This can contribute to the symptoms of a blocked vein in the leg. To prevent these complications, it is recommended to follow these measures:
1. Wear comfortable shoes that are not too tight or consider taking off your shoes during the flight. This helps promote better blood flow.
2. Regularly move your ankles and legs while seated or take short walks in the cabin to improve blood circulation. Avoid remaining in a position where the legs are pressed or crossed for prolonged periods. Additionally, refrain from using sleeping pills, as they can cause deep sleep, making it difficult to notice if the legs are being compressed for an extended period.
3. Stay hydrated by drinking enough water during the flight. It is advisable to limit the consumption of alcohol and coffee, especially during long-duration travel, as they can lead to increased urination and vascular dilation, potentially contributing to the development of blood clots in the legs.
4. Patients with a history of venous thromboembolism or blood clots in the lungs should take preventive medication before traveling, as prescribed by their healthcare provider.
Other patients who should not travel by air
1. Patients with certain eye diseases, such as retinal detachment within the past 3 weeks, recurrent glaucoma or recent eye surgery within the past month, and corneal inflammatory disease where the wound has not completely healed.
2. Individuals with sinus disease or acute ear infections.
3. People who have undergone ear surgery within the past 3 months.
4. Patients with anemia and a blood concentration of less than 10 g/dL should avoid air travel as the available oxygen may not be sufficient for their body’s needs.
5. Individuals with medical conditions that require prohibited medical equipment on board the aircraft.
6. Patients with infectious diseases in their contagious stage (e.g., chickenpox, measles, mumps, whooping cough, shingles).
7. Individuals with AIDS and serious complications.
8. Diabetic patients who are unable to control their blood sugar levels should refrain from traveling. Those with proper sugar control should inform the airline in advance to arrange for diabetic meals. Medications should be carried on board the plane, and if using injection equipment, a medical certificate must be provided. It is important to maintain meal and medication times based on the departure station’s time and adjust accordingly to the new time at the destination.
9. People who have recently had an accident and are still awaiting assessment of complications or undergoing treatment.
10. Patients who have undergone surgery within the past 7 days.
11. Individuals with recent splinting should have the splint removed before traveling.
12. Patients with large wounds or severe burns that are not healing well.
13. Terminally ill patients who may experience deterioration during travel.
For clients with peanut allergies:
If the airline has been informed in advance, they can make appropriate arrangements to accommodate passengers with peanut allergies, including providing special meals and taking necessary precautions to ensure their safety. It is advisable for passengers to carry documentation of their allergy medication usage and wear a hospital wristband indicating their peanut allergy. This will help the flight attendants recognize the allergy and provide prompt assistance when needed.
During the flight:
People with heart and respiratory problems
- It is important to adequately prepare and carry sufficient medication for your regular use when traveling. Keep all medications in your carry-on bag, particularly those used to address emergency symptoms such as painkillers, bronchodilators, and sublingual lozenges for relieving chest pain. Also, carry injections to manage blood sugar levels as recommended by your doctor, as well as a subcutaneous injection for acute allergic reactions (Epipen).
- For asthma patients, especially those with mild symptoms, ensure that your medication, particularly inhalers, is readily available during the flight.
- If you require oxygen during your flight, make sure to notify the airline in advance by completing a medical information form that includes your current clinical condition and the reasons for needing oxygen. Submit the form to the airline for approval, which may take 3-5 working days depending on the airline’s procedures.
- To prevent dehydration, drink plenty of water during the flight. Staying hydrated helps dissolve phlegm and keeps your lungs clear, especially in low humidity conditions in air-conditioned environments.
Patients with brain diseases or abnormal cerebrovascular conditions:
– Uncomplicated or stable stroke at least 2 weeks before the trip The treating physician should consider requesting additional oxygen on board.
Patients with gastrointestinal diseases:
– Patients who have had the colon opened in the abdomen (colostomy) should prepare to bring more colostomy bags than the usual amount for replacement during travel.
Patients with venous thrombosis in the legs:
This condition is known as deep vein thrombosis (DVT), which can occur when sitting in cramped seats for extended periods, leading to poor blood flow from the legs to the heart. This can result in swollen feet and legs and, in some cases, the development of blood clots in the legs. To prevent DVT, it is recommended to follow these measures:
1. Wear comfortable shoes that are not too tight or consider taking off your shoes during the flight to promote better blood flow. Additionally, move your ankles and legs regularly or get up and walk around when permitted by the airline staff. It is advisable to change your sitting posture regularly and, with permission, alternate between flexing and extending your legs. Periodically wiggling your feet, such as every 30 minutes, can also help stimulate blood flow.
2. Avoid sleeping in a position where the legs are pressed, as this can contribute to prolonged compression and reduced blood flow. It is not recommended to use sleeping pills during the flight, as they can induce deep sleep and make it difficult to notice if the legs are being crushed for an extended period.
3. Stay hydrated by drinking enough water during the flight. Limit the consumption of alcohol and coffee, particularly during long-duration travel, as they can cause increased urination and vascular dilation, potentially increasing the risk of blood clots in the legs.
4. For patients with a history of venous thromboembolism or blood clots in the lungs, it is crucial to take preventive medications as prescribed by their healthcare provider before traveling.
5. If you are at high risk of developing deep vein thrombosis, it is advisable to consult your doctor for personalized advice and treatment options. They may recommend measures such as using special compression stockings, taking aspirin (a blood thinner), or anticoagulant medications.
- Maintain personal hygiene and prevent infection by frequently washing your hands with soap and water. Carry hand sanitizer gel for added protection. Maintain a social distance of more than 1 meter and wear a hygienic mask at all times, following appropriate guidelines.
– According to the announcement of the Ministry of Public Health of Thailand, subjecting hospitals and vehicles It’s a non-smoking area. By requiring the area and all areas both inside and outside the building Whether there is a fence or not, including a distance of 5 meters from the entrance-exit of the place. The hospital would like to inform you that Smoking is not permitted in hospitals and in vehicles.
Note: Smoking includes smoking and e-cigarettes.
Section II: Pre-operative Preparation
- Please inform the doctor before surgery. if you have a medical condition that you are taking and/or you have had surgery before the trip.
- If you are taking anticoagulants like aspirin, Persantin®, Ticlid®, Plavix®, warfarin, Orfarin®, heparin, and Fraxiparine®.You must be consulted by a medical practitioner before undergoing surgery.
- Herbal supplements, and vitamins, especially vitamin E, stop these supplements at least one week before the surgery or as recommended by your doctor.
- If you smoke and drink alcohol regularly, please stop for at least one week before the surgery to reduce the chances of complications.
- Please inform your physician of any underlying diseases: cardiovascular disease/diabetes/high blood pressure/asthma/cancer/or allergic to any medications.
- In case of knee replacement surgery, you are requested to undergo a dental check-up to reduce the chances of infection.
Section III : Conditions for infectious disease screening
- Please inform your physician of any underlying diseases: cardiovascular disease/diabetes/high blood pressure/asthma/cancer/or allergic to any medications.
- COVID-19 (SARS-CoV II) would like to inform you that COVID screening depending on the symptoms and other unpredictable complications But if you are found to be infected with COVID-19, you will need to receive treatment for COVID-19 as well, which may result in complications that may be severe and lengthen your hospital stay. And the cost of hospitalization is inevitably required to increase with such treatment.
- Chicken Pox
- Tuberculosis
- Measle
- Rubella
- Diphtheria
- Pertussis
Section IV : In case of an adverse event
- You must have an insurance policy showing medical coverage in Thailand covering COVID-19 for an amount not less than US$10,000.
- before the trip You should have a physical examination by your personal physician. Including a travel certificate (Medical Fit-to-fly) or other medical certificates that certify that you can travel safely. by physical examination This should be done within 72 hours of travel.
- You should communicate to the airline to prepare According to the advice of the owner’s physician or specified in the travel certificate or medical certificate to prepare for potential emergencies during the flight on the airline
- In case of postpone of treatment due to any uncontrollable cause or can be avoided, such as restricting travel in and out of the United Kingdom, Thailand and may cause the treatment to be postponed Ratchaphruek Hospital has a guideline to advise on comorbidity that may occur to you by the hospital’s doctors communicating via video call. (Provided that you have already signed a consent to receive this service before the trip)
- When you are able to travel to the United Kingdom of Thailand and can be treated at Ratchaphruek Hospital You may have a diagnosis. or repeated medical screening Because the results of the original diagnosis that was submitted earlier may change. which results in additional expenses in this section However, such re-examination will depend on the opinion of the doctor who directly supervises you.
- In case you want Ongoing care after arriving at the destination airport able to coordinate to Ratchaphruek Hospital through the following channels:
- Via Email: [email protected] , [email protected]
- Official Website: www.rph.co.th
- Official Line OA: @rphline
- by phone at phone number
- (66) 84 462 8708 (International Marketing Manager)
- (66) 333 555 ext. 4056 (International Marketing Manager department number)
- (66) 43 333 555 ext. 2117 (Emergency Department)
- (66) 86 458 4703 (In-charge of the Emergency Department)
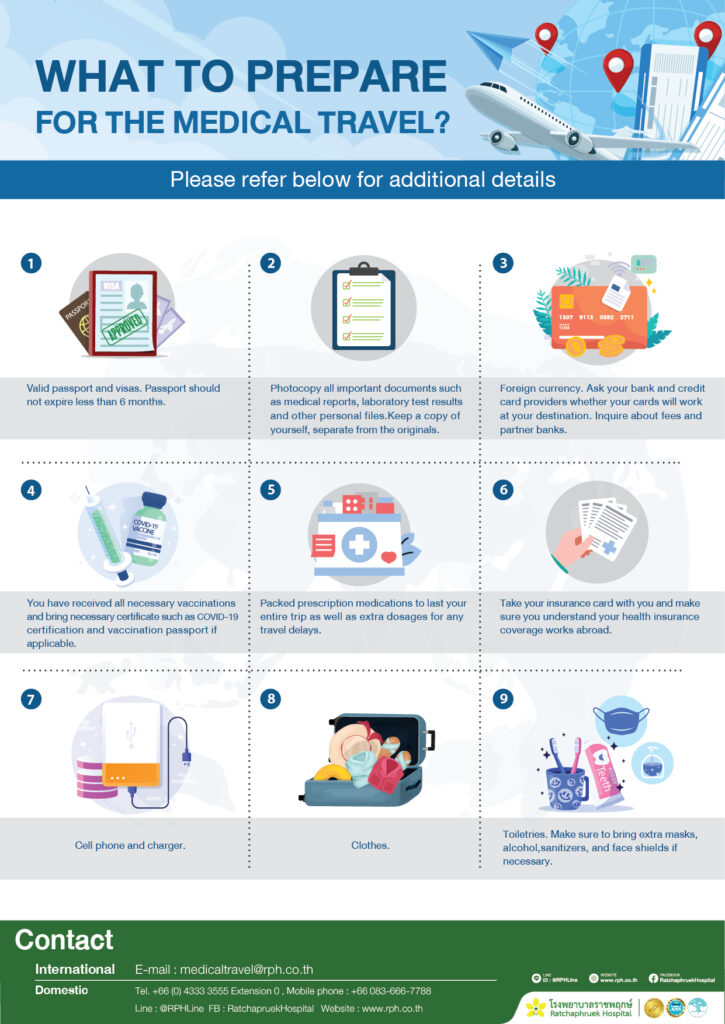
WHAT TO PREPARE FOR THE MEDICAL TRAVEL?
**Please refer below for additional details:
- Valid passport and visas. Passport should not expire less than 6 months.
- Photocopy all important documents such as medical reports, laboratory test results and other personal files. Keep a copy of yourself, separate from the originals.
- Foreign currency. Ask your bank and credit card providers whether your cards will work at your destination. Inquire about fees and partner banks.
- You have received all necessary vaccinations and bring necessary certificate such as COVID-19 certification and vaccination passport if applicable.
- Packed prescription medications to last your entire trip as well as extra dosages for any travel delays.
- Take your insurance card with you and make sure you understand your health insurance coverage works abroad.
- Cell phone and charger.
- Clothes.
- Toiletries. Make sure to bring extra masks, alcohol, sanitizers, and face shields if necessary.
IPAP
Pre-arrival
- Healthcare at Ratchaphruek Hospital
- Safety and Security
- Immigration and Customs
- The Entry into Thailand
- Travel Advice and Support
- Travel Checklist
- Patient’s Rights and Patient’s Responsibilities
- Special Announcement
- Safety Protocol (Infographics)
- Package for Medical Travel
- Telemedicine
- Accredited Standard & Awards
Arrival
- Ratchaphruek Airport Representative
- Meet and Greet at Khon Kaen airport
- Map to Ratchaphruek Hospital
- Safe and clean
Admission
Departure
- Pre-Discharge Plan
- Discharge Plan
- Follow Up
- Level of Satisfaction for Health Experience
- Patient Experience
 English
English 
 Hotline 043-333555
Hotline 043-333555