1) Basic information
There are different types of breast cancer surgery. Total mastectomy and/or total mastectomy and modified Radical Mastectomy are other popular procedures that involves removing the breast tissue, nipples, and birthmarks. Or perhaps the whole breast and skin of the breast, or may also remove the lymph nodes under the armpit.
1.1 Total Mastectomy (Total or Simple Mastectomy) is the removal of the entire breast including the skin above the lump and nipple but without removing the axillary lymph nodes. It is most often performed in cases where the lymph nodes under the armpit cannot be felt. A Radiologist will usually inject a contrast medium into the lymph nodes under the armpit to test (sentinel lymph node biopsy) to see if the cancer has spread to the lymph nodes. (See “Sentinel lymph node” guide.)
1.2 Modified Radical Mastectomy is the surgical removal of the entire breast including the skin above the cancer. Also Including the nipples, the base of the mammary glands, the axillary lymphatic tract but leaving the pectoral muscles intact. Patients may be at risk of postoperative swelling of the arm. Therefore, doctors often recommend that patients do continuous exercise to prevent joint pain and the shoulder joint stiffens and the arm becomes swollen. Patients undergoing a mastectomy will feel unbalanced and the surgical area will be tight. The muscles of the shoulders and arms become tight and feel weak. This problem will disappear by (doing arm and shoulder exercise) as recommended by the doctor. Sometimes surgery may cause arm numbness or a burning sensation in the chest, under the armpits, shoulders, and upper arms. These symptoms will disappear within 3-4 weeks but may cause that arm to swell due to poor lymph circulation.
2) Intervention Options
2.1 Breast conserving surgery
Breast conserving surgery followed by radiotherapy depends on the stage of the disease and the physician’s discretion.
2.2 TRAM flap (Transverse Rectus Abdominis
Myocutaneous flap) Total mastectomy and breast reconstruction TRAM flap (Transverse Rectus Abdominis Myocutaneous) is divided into 2 types:
2.2.1 Immediate breast reconstruction
2.2.2 Delayed breast reconstruction
2.3 If cancerous masses are found, the most appropriate treatment method is surgery. After surgery, there are 3 well-established concomitant treatments, each depending on the stages of the disease, the patient’s condition and consultation with a medical specialist. These three methods are as follows.
2.3.1 Radiotherapy
2.3.2 Taking hormonal drugs
2.3.3 การใช้ยาเคมีบำบัด Chemotherapy
3) Risks and side effects of treatment
3.1 General Risks
1. For general pain and pain at the surgical site, the patient can take a painkiller to relieved pain.
2. In the case of prevention of Infected wounds, difficult wounds, bleeding conditions around the surgical wound and complications from general anesthesia please be aware that clinical team of doctors and nurses, and support persons will take care and keep the occurrence of such conditions to a minimum.
3. Tension or discomfort in the shoulder, neck, chest or arm may occur for a period of time when the initial pain subsides. The care team will give appropriate advice according to the individual condition so that the patient can begin exercise. When exercise begins regularly, this feeling will improve.
4. Numbness in the chest, shoulders, and underarms is caused by nerves in the underarms or under the armpits being cut or electrified. The symptoms last for about 2-3 months.
3.2 Specific Risks
1. Tension or discomfort in the shoulder, neck, chest or arm may occur for a period of time once the pain subsides. The care team will give appropriate advice according to the individual condition so that the patient can begin exercising. When exercise begins regularly, this feeling will improve.
2. Numbness in the chest, shoulders, and underarms is caused by nerves in the underarms or under the armpits being cut or electrified. The symptoms last for about 2-3 months.
3. Monitoring lymph or waste buildup in the wound after surgery The care team will regularly monitor the number of colors and appearance of waste as well as the operation of the vacuum vent bottle. If there are abnormal symptoms or the amount of waste is greater than normal, the doctor will immediately proceed with medical treatment according to medical standards.
4. In the case of lymph node removal surgery in the armpit, there may be swelling of the operated arm due to blocked lymphatic channels. The care team will instruct the patient to be careful of pressure on the arm, exposure to heat, use of the mastectomy arm, use of excessive force, or lifting heavy objects. Do not draw blood, receive an injection, or measure blood pressure with that arm. Be cautious of arm injuries and see your doctor If there is a suspected infection in the area.
4) Preparation before surgery
1. Consuming from five food groups, including rice, meat, vegetables, fruit and water, is the key to helping in healing and faster patients recovery.
2.Patients with underlying diseases that are at risk from general anesthesia such as diabetes, high blood pressure, heart disease, kidney disease, and lung disease need to be controlled to a normal condition in order to prevent intraoperative and postoperative complications.
3.Various laboratory tests will be requested by the doctor with consideration of the results in advance in order to assess the patient’s readiness for surgery.
4. Once the patient and relatives have been completely informed regarding the disease, the surgical procedures, and the cost of treatment, they must sign a consent form covering the surgery, general diagnostic procedures, agreement to undergo surgery and acknowledge the anesthesia use consent form. If the patient is in a condition causing them to be unable to express the intention to give consent normally or the patient is under 20 years of age, a parent or legal representative must give consent on behalf of the patient.
5. Prepare your mental state to try to reduce anxiety, get enough sleep, create a feeling of hope and encouragement for yourself and for relatives for their support as well. If you have any apprehension or don’t understand anything, ask your doctor and the caregiver team.
5) Preoperative preparation
The day before surgery
1. Take care of general body hygiene, take a shower, wash your hair, remove nail polish, cut your fingernails and toenails.
2. Clean the skin in the surgery area. In some cases the doctor will consider shaving the breast and armpit hair on the side of the surgery to prevent infection.
3. In the case of surgery that requires general anesthesia, the patient must abstain from food and water after midnight before the surgery day or at least 6-8 hours before the surgery in order to empty the stomach.
4. Practice effective breathing and coughing to prevent respiratory complications after surgery.
4.1. Practice Efficient breathing in order to help the lungs expand well and improve blood circulation. Here are steps to follow.
– Stay in a semi-sitting position to relax your abdominal muscles and allow your chest to fully expand. Place your hand lightly on your belly and inhale slowly through your nose to fully expand your lungs, and exhale slowly through the lips (the belly will curl in). Practice doing this about 5 times to get used to it.
4.2. Effective coughing is to expel phlegm from the respiratory tract
– After 3-5 effective breaths, cough from the depths of your lungs by holding your breath, after inhaling and coughing out vigorously.
Morning day of surgery
1. Take a shower to purify your body again to make your body clean and fresh.
2. Remove valuables, dentures, fake hair (Wig), contact lenses, and leave them with relatives.
3. Urinating before going to the operating room
4. Intravenous medications may be administered for relaxation at the physician’s discretion.
6. Postoperative care
Patients will be closely monitored by nurses throughout the first 24 hours after surgery to keep them safe from falling off the bed. As well, observation of various uncomfortable symptoms such as wound pain, excretion, and administering intravenous solutions, taking care of the tube or drain from the wound If the doctor considered one necessary. In addition, there are things that patients will take care of, including observation and being cautious. Relatives can help as follows.
1. After the surgery, lie down and raise the operated arm to 45 degrees using a pillow under the arm to improve blood circulation and prevent arm swelling. Do not measure blood pressure, give fluids, or inject drugs both through the muscles and the arteries of the operated arm to prevent infection and swelling of the arm.
2. This surgical wound is covered with a bandage. The patient must be careful not to get wet. If there is a lot of blood seeping into the bandage, the nurse must be notified immediately.
3. When the patient has pain at the surgical site, the nurse will administer pain medication to be taken every 4-6 hours or may give intravenous pain medication according to the doctor’s treatment order.
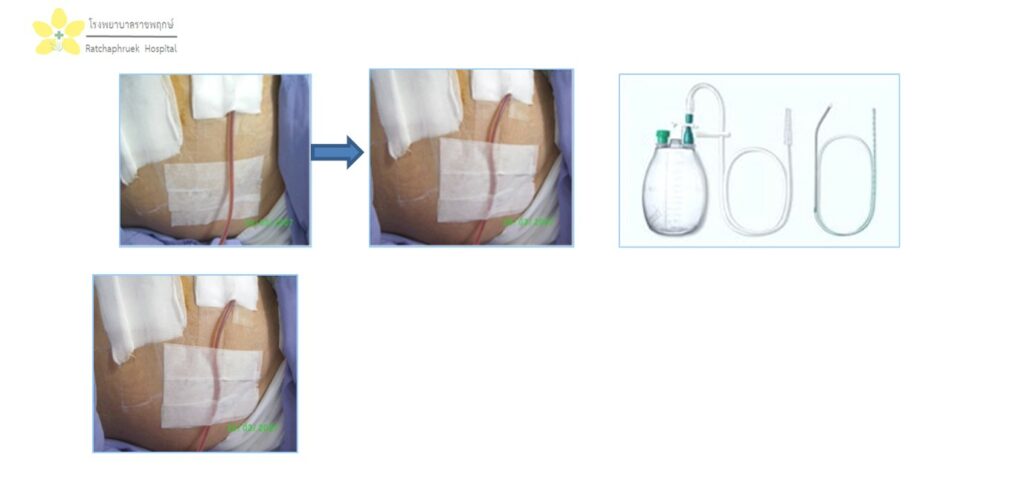
4. Most surgical wounds will have a drain tube. Take care not to break, bend, leak or slip from the original position and always watch the operation of the tube or drain tube to prevent it from being blocked and place the drain bottle below the surgical incision.
5. Observe complications after surgery, such as swelling, pain, more surgical wounds, fever, stiffness, swollen joints, frozen shoulder, etc. These symptoms occur, promptly notify the care team or if you return home and if you have an abnormality, you need to see a doctor immediately.
6. Perform physical exercises after the pain subsides as recommended by the care team to rehabilitate the body and prevent frozen shoulder joints, especially in the case of having removed the lymph nodes under the armpit.
7. It is recommended to eat all 5 food groups, especially protein such as milk, meat, eggs, nuts to help the wound heal faster and strengthen the body after surgery.
8. Encourage the patient to resume normal daily activities.
9. Providing care for receiving antibiotics according to the doctor’s treatment plan in entirety.
10. Give the relatives an opportunity to participate in encouraging, taking care of, listening to the feelings or discomfort of the patient, including finding ways to help patient recover physically and mentally and return to normal life as soon as possible.
Radivac drain Caring for the drain connected to the Redivac drain vacuum flask
In the case of an inserted drainage tube from the wound, the amount of discharge excreted from the wound will be determined by the doctor. If the total amount within 24 hours is less than 50 cc per day, then the doctor will remove the tube drain from the wound and allow the patient to go home. But in some cases, there may still be more discharge, so the doctor may let the patient carry drain tube home. Instructions for caring for the drain hose are as follows.
- Take care that the drain tube does not fold or bend.
- Hold on to the drain tube firmly, do not tug pull aggressively.
- Always ensure that the drain bottle is in a vacuum system. (Notice the top rubber stopper shrinks)
- Observe the color, appearance, amount of secretion and record it every day.
If there are any abnormal symptoms, you can contact Ward 6. Telephone 062-215-5957 or Ward12. Telephone 066-121-0910 at any time, or if urgent, you need to see a doctor at a hospital near your location. Abnormal symptoms that require urgent medical attention, such as
- More wound pain, fever, red swollen wound
- Airless bottle not working or the amount of discharge in the bottle amounts to ¾ full.
How to apply plaster to prevent the drain tube from sliding off.
Appointment and follow-up.
- Treatment follow-up.
- Travel to see a doctor in person at Ratchaphruek Hospital
- Treatment follow-up via telemedicine (which requires prior consent)
- (With a history of treatment for the patient)
2. If the patient has returned to their own country and has abnormal symptoms such as increased surgical wound pain, fever, swollen and red surgical wounds, they can contact a physician at Ratchaphruek Hospital via WhatsApp/ LINE/ Video call/ Microsoft Team/ Zoom where they were informed prior to the trip for advice. Or urgently go to see a doctor at a local hospital for a medical examination.
3. It is advisable to undergo periodic physical examinations according to the program to check for recurrence of breast cancer.
4. Advise patients to strictly follow the doctor’s instructions for the best treatment results.
5. Patients are advised to examine the remaining breast regularly at least once a month. If abnormalities are found, the patient should see a doctor immediately. In which the occurrence of breast cancer on the other side may have a chance to occur. Following this program will help detect anomalies more quickly.
For more information, please contact the surgery department at 084-027-2076.
In-Patient Department, 6th Floor Tel. 062-215-5957
In-patient Department, 12th Floor Tel. 066-121-0910
WEBSITE www.rph.co.th
LINE ID: @RPHLine
 English
English 
 Hotline 043-333555
Hotline 043-333555